WARNING - This page contain medical photos and is only suitable for people aged 18-yrs and older
Breast Reconstruction
What is breast reconstruction?
Breast reconstruction is done after a mastectomy, which is the removal of a breast. This surgery is typically needed due to breast cancer treatment or to prevent cancer in patients at high genetic risk. The goal is to recreate the breast's natural shape after removal. It's important to note that post-mastectomy breast reconstruction is not a cosmetic procedure and differs from breast augmentation, which is for enlargement.
Is Reconstruction the same as Breast Enhancement/Augmentation?
Breast reconstruction after mastectomy is different from breast enhancement. Breast enhancement is a cosmetic procedure to increase breast size using implants, which push the breast forward. Dr. Green does NOT perform breast enhancements; you would need to see a specialist cosmetic plastic surgeon for that.
What is the aim of the reconstruction?
Breast reconstruction is done after a mastectomy as part of breast cancer treatment. The goal is to restore a breast shape that you are happy with. Your natural breast shape is the ideal, and it can be enhanced with cosmetic techniques. However, recreating a breast that looks exactly like your natural one is challenging.
What are the different types of breast reconstruction?
In general terms there are two broad categories of breast reconstruction. These include:
Implant Based Reconstruction
Implant-based reconstruction is the most common type of breast reconstruction. Here, the outer skin is kept after removing breast tissue, called a subcutaneous mastectomy. An implant, tailored to your breast shape and size, is then placed inside. With modern techniques, good results can closely mimic your natural breast. This method works best for smaller breasts without droop.
Implant reconstruction can often be done right after surgery, known as immediate implant reconstruction. Modern implants are safe and durable, adding little extra time to the operation and recovery. However, implants may not feel completely natural, can get cold when swimming, and generally need to be replaced every 10 years.
Right breast - post nipple sparing mastectomy with immediate implant reconstruction
Left breast - Natural breast
Autologous - Tissue based
An autologous reconstruction uses your own tissue to rebuild the breast, usually taken from the lower abdomen like in a tummy tuck. Examples include TRAM (Transverse Rectus Abdominis Myocutaneous) flap and DIEP (Deep Inferior Epigastric Perforator) flap. The benefits are that the tissue is natural, adjusts with your body weight, and provides a flatter lower abdomen. However, you need enough tissue in your lower abdomen for this procedure. The surgery is extensive with a longer recovery time and has two areas to manage afterward. Options are limited if complications arise. This method is not suitable for smokers or those with vascular disease, and it cannot be performed alongside a mastectomy if radiation is anticipated. Keeping the nipple is also not possible.
Right Breast - Autologous DIEP Flap with nipple tattoo
Left breast - natural breast
What is the best type of reconstruction?
Each type of breast reconstruction has pros and cons, and none is the best for everyone. The right choice depends on your body shape, breast shape, and cancer treatment. A good reconstruction can restore shape and create an attractive breast. There are various options, and the best one varies based on several factors: your expectations, comfort with surgery, breast cancer treatment (especially if radiation is needed after mastectomy), body shape, and smoking status.
Expectations
It's important to manage expectations. Not all breasts are suitable for reconstruction, and your natural breast is the best. Understanding the surgery involved for each type of reconstruction is crucial when making your decision. Discuss your options with Dr. Green to see what works for your body type, as not all options may be available to you.
Extent of surgery
Breast reconstruction involves significant post-operative care, and being informed is crucial. An implant-based reconstruction typically lasts 2-3 hours for both breasts, with most patients staying in the hospital for 2-4 days and going home with drains and antibiotics. Full recovery usually takes about 6 weeks, and this type of reconstruction is generally not very painful, so heavy painkillers are often unnecessary.
In contrast, autologous reconstruction methods like TRAM or DIEP are more extensive procedures. They usually require a hospital stay of 6-12 days, with the surgery lasting 6-12 hours. The minimum recovery time before returning to normal activities is also 6 weeks, and only patients deemed fit can undergo this type of reconstruction.
The Impact your cancer treatment has on reconstruction
When choosing a reconstruction method, it is crucial not to postpone your cancer treatment. After treatment, you may need chemotherapy or radiation, which are vital for a good outcome. Autologous reconstructions typically happen after all cancer treatments are finished because recovery takes too long to delay chemotherapy. If radiation is likely after your mastectomy (especially with larger cancers or multiple lymph nodes), an autologous reconstruction should be delayed since radiation makes reconstruction more difficult. Immediate reconstruction is usually not recommended due to potential complications. Implant reconstruction can be performed before radiation, but if complications like infection arise, the reconstruction may need to be halted, and only a simple mastectomy scar would remain to avoid delaying cancer treatment.
Smoking
Smoking greatly increases the risk of complications after any surgery, especially breast reconstruction. If you smoke, autologous reconstruction is not an option due to a high risk of major complications. For implant-based reconstruction, you may still qualify, but there will be limits. Any complications could lead to the removal of the implant and a simple mastectomy scar. Smokers are less likely to preserve the nipple, and you may need a staged approach using a temporary tissue expander.
Can a reconstruction be done immediately after my mastectomy?
All patients having a mastectomy should discuss their reconstruction options with Dr. Green. Most can have immediate reconstruction, especially with implants. Autologous reconstruction usually happens after completing treatment. For patients at high risk due to family history or gene mutations, there’s no rush to start chemotherapy, making autologous reconstruction an immediate choice. If reconstruction might delay cancer treatment or poses a high infection risk, it will be postponed. More cancers are now treated with chemotherapy before surgery (neoadjuvant chemotherapy). If you smoke, stopping for at least 6 weeks can expand your reconstruction options.
What is an Immediate Direct Implant Reconstruction?
Dr. Green commonly performs this type of reconstruction, which allows for a quick recovery that usually doesn’t delay cancer treatment. In Direct Implant reconstruction, after a mastectomy, an implant tailored to your size is placed above the chest muscle and beneath the skin, known as Pre-Pectoral Direct Implant reconstruction. Previously, implants were placed under the muscle, but that approach is no longer used due to complications and pain.
Pre-pectoral reconstruction is generally not very painful and requires a hospital stay of 2-4 days. Patients leave with surgical drains that are removed during the follow-up visit. Most do not need strong pain relief.
Modern implants can achieve a shape similar to your natural breast. The implant cannot be placed directly under the skin; it must be wrapped in a special covering called a Dermal Matrix. Dr. Green uses Flex HD, a high-quality human tissue matrix that helps your tissue grow around the implant naturally, without artificial mesh.
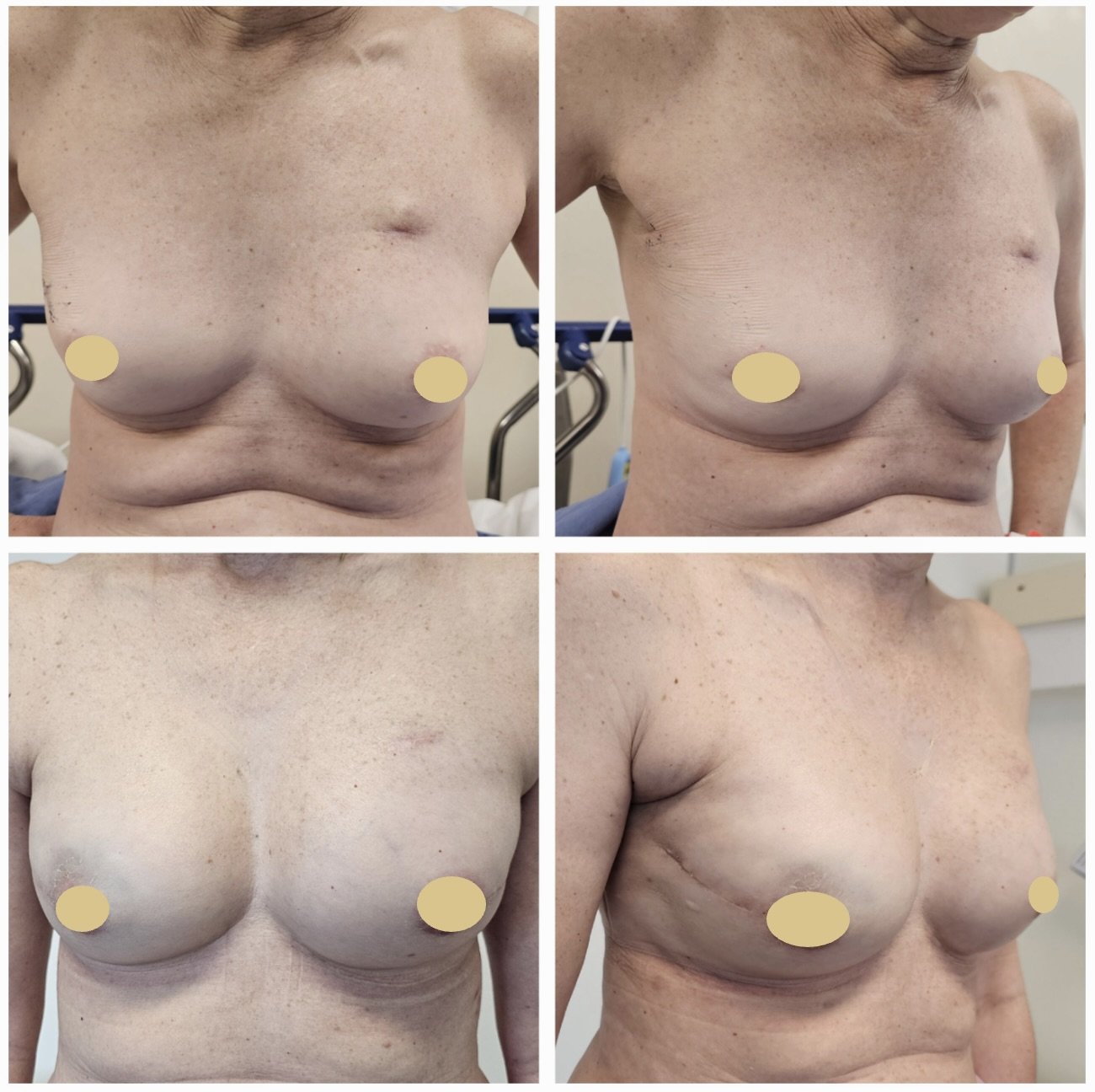
Pre-op photo top, Post-op photo bottom
Image 1 - Left sided nipple preserving mastectomy and immediate pre-pectoral reconstruction, natural right breast
Pre-op photo top, Post-op photo bottom
Image 2 - Left sided nipple preserving mastectomy and immediate pre-pectoral reconstruction, natural right breast
Pre-op photo top, Post-op photo bottom
Image 3 - Bilateral nipple preserving reconstruction, following previous right lumpectomy - Found to be BRCA1 carrier during chemotherapy
Breast Implant wrapped in FLex HD for Direct Implant Reconstruction (DTI)
When is a two staged approach needed?
A two-stage approach is used in certain cases, such as for higher-risk patients (like smokers or those needing radiation) or for those wanting a larger breast. Most of Dr. Green's surgeries involve Direct to Implant (DTI) reconstruction. If DTI isn't possible, a two-stage method with a tissue expander may be needed.
This form of reconstruction is performed in two stages:
Stage 1 – Placement of the tissue expander - empty or partially filled
Stage 2 – Switching of the expander to permanent silicone implant.
Stage 1 – Placement of expander and expansion
The expander is initially put in empty or only partially filled. It sits under the breast skin, in front of the chest muscle, and is covered by a Dermal Matrix. The goal is to completely cover the expander with this material. After the wounds heal, the expander is gradually filled with saline, stretching the skin to make room for a permanent implant in the next stage. The time this takes depends on the desired size and how much fluid was added during surgery. Expansions are done in the office, usually adding 50-100ml every 1-2 weeks. A tissue expander is beneficial because it can be deflated if there are any healing issues, relieving pressure on the wound and helping it heal better.
Stage 2 – Placement of permanent implant
Once the expander is fully inflated, it will feel hard and may stick out more than the final implant. This will be fixed in the second stage, which is scheduled after all your breast cancer treatment is finished. You need to wait at least three months after expansion to make sure the area is fully healed. The second surgery is quick; it involves reopening the scar, removing the expander, and placing a permanent silicone implant that is custom-shaped for you and feels softer and more natural. Small adjustments to the implant's position can also be made during this operation.
TOP IMAGE - Right breast had a previous mastectomy with No reconstructionUnderwent an initial tissue expander reconstruction Tissue Expander is now fully expanded
BOTTOM IMAGE - Right has undergone second stage reconstruction with Expander being removed and new permanent implant placed.Left - Immediate nipple sacrificing subcutaneous mastectomy and immediate Pre-pectoral Direct Implant reconstruction at same time as right second stage
Are Breast Implants Safe in breast Reconstruction?
Yes, breast implants are very safe and durable. It takes significant force to rupture them, such as in car accidents or certain sports. Implants are made of silicone, which is safe for the body and does not cause inflammation if ruptured. Long-term ruptures can lead to shape changes and discomfort due to a thick capsule that forms around the implant, but this can be managed by removing the capsule during replacement. Implants require care and usually need to be replaced every 10 years, though they can last longer with proper maintenance and minimal trauma.
Breast Implant Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) is an extremely rare condition linked to textured breast implants. The microtextured implants used in reconstruction have the lowest risk, estimated at about 1 in 14,000. This condition usually causes significant fluid swelling 1 to 8 years after implantation. Treatment involves removing the implant and the surrounding tissue capsule. Although it is very rare, we will monitor it during your cancer follow-up. For more information on BIA-ALCL, please check the Therapeutic Goods Administration.
Breast Implant Illness (BII) is a growing concern where many women who have had breast augmentation report various non-specific health issues. Patients often undergo extensive tests over several years without finding a clear cause. Some choose to reverse their breast augmentation and have the implants removed, reporting symptom improvement afterward. Although no medical link has been established between breast implants and these symptoms, more women are sharing their experiences online. Data on this condition is being collected, and increasing reports suggest many feel better after removal. Dr. Green has significant experience in helping women with BII symptoms, and many report improvements. However, many women with implants experience no problems at all. Patients who are concerned about their implants impacting their health should discuss potential benefits of removal with their surgeon. It's important to note that most BII cases come from breast augmentation, not breast reconstruction. Dr. Green does not perform breast augmentation surgery.
Potential complications
All surgeries can have complications. While these are not planned, some can be minor while others may be severe and require additional surgery. Below is a list of common complications related to breast reconstruction, though it is not exhaustive. With implant reconstruction, artificial materials are used, and your body may try to reject them. Although precautions are taken, sometimes the reconstruction can fail, leading to a poor result that necessitates more surgery.
It's important to have realistic expectations. Your natural breast is unique, and once it is removed, it's challenging to create an identical one. Dr. Green will stress the importance of understanding what is achievable. Here are some potential complications associated with implant reconstruction:
More Common - up to 10% of cases
Seroma – fluid collection.
‘Dog ears’ on wound needing correction.
Numbness over chest wall.
Visible Rippling of implant - especially if very thin
Uncommon - up to 5% of cases
Wound edge necrosis (dying skin).
Nipple necrosis (dead nipple needing excision).
Wound infection.
Infected implant – needing removal.
Migration on implant
Poor cosmetic result.
Painful capsular contracture
Device migration, rotation, flipping
Implant rupture
Rare but important - less than 1% of cases
Anaesthetic complications.
Very poor cosmetic result.
Implant associated Anaplastic Large Cell Lymphoma (BIA-ALCL) - 1:14000
Breast Implant Illness - non-specific symptoms possibly related to breast implants
To Be aware of:
Replacement of implant after 10 years is likely